The purely economic case for investing in Health for All
This blog is ahead of the forthcoming Working Paper:
Vallès-Codina, O. (2022, forthcoming). “The purely economic case for investing in health for all in lower- and upper-middle income countries: input-output and network analysis of their industrial ecossytem”. UCL Institute for Innovation and Public Purpose, Working Paper Series (IIPP WP 2022-03)
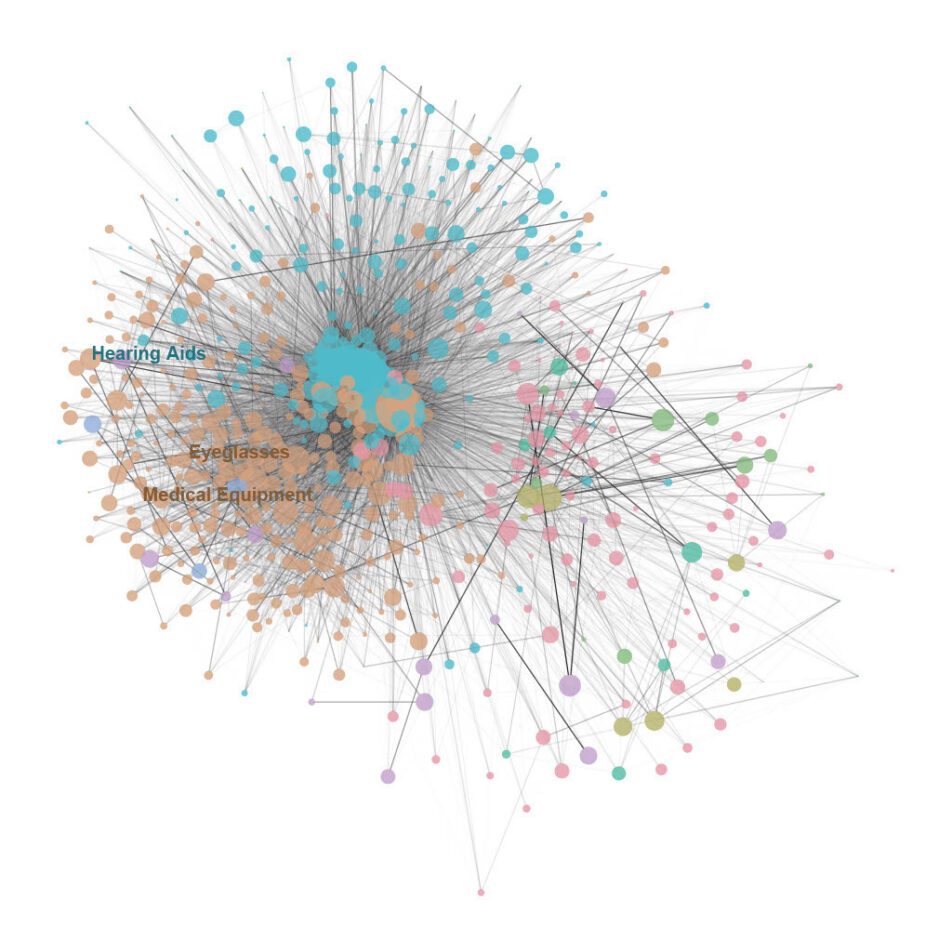
Visualization of the Mexican network of production of Assistive Technology
The purely economic case for investing in Health for All
Complete physical, mental, and social well-being, that is, health, is a fundamental human right - to be guaranteed by universal health coverage. The severe economic and health crisis provoked by the ongoing Covid-19 pandemic demonstrates that unless global health systems are governed for the common good, many people remain excluded from their benefits, exacerbating existing inequalities in the form of precarious income insecurity and underfunded and stretched health systems after decades of austerity policies, further incurring in subsequent unacceptable economic and health costs (WHO 2021a). Contra what many believe and in agreement with our latest research (Vallès Codina 2022), the Covid-19 pandemic revealed that there is no trade-off between investing in our health systems and economic growth. Instead, health and the economy are, in fact, fundamentally interdependent: not only health is in itself a key economic sector, but also a crosscutting issue underlying all economic activity, with a special emphasis on the basic performance of labor that is essential for the economy (WHO 2021a). For the WHO Council on the Economics of Health for All, “health is critical to the resilience and stability of economies and societies worldwide” (WHO 2021a).
However, both for-profit commercial initiatives and charitable efforts led by non-profit organizations are insufficient to deliver health for all and its substantive economic benefits (WHO 2021a). In this context, policy makers are increasingly embracing market shaping: the idea of using industrial and innovation policy to tackle the ‘grand challenges’ facing modern societies, among which the transition to a low-carbon economy and health for all are the most critical. Designed to be transformative, market shaping aims to reduce long-term demand and supply imbalances, reduce transaction costs, and increase market information, requiring the participation from countries, donors, procurers, service providers, end users, and beyond, in line with a unified strategy (USAID 2014). A market-shaping role for policy would enable shifting not only the rate, but also the direction of economic growth, namely towards broader notions of public value creation driven by public purpose instead of private profit (Kattel et al 2018). We need not only more, but also better finance, immediately creating fiscal space by reversing the ruling austerity approach and delivering a specific direction of investment set under a long-term, mission-setting perspective, coupled with the synergic governance of public and private finance (WHO 2021b).
While investment –either public, private, and non-profit- must be oriented in the long run towards the grand challenges that modern societies face today, our research clearly shows that the returns of mission-oriented investment are in fact immediate, involving rapid positive spillover effects in public revenue, output, and employment in the short run, as well as deep structural changes to the economy that move it towards serving the needs of the many and not the few (Vallès Codina 2022). Across health sectors, market shaping has demonstrated its potential to enhance national governments’ or donors’ value-for-money, diversify the supply base, and increase reliability – ultimately increasing product and service delivery access for end users (Savage 2021). The successful implementation of market shaping in a variety of contexts, including global health, has led many practitioners to hypothesize that it could also be applied to assistive technology markets.
In order to properly deliver health for all, assistive technology is critical. Global commitments such as the UN Convention on the Rights of Persons with Disabilities recognize it as a human right. Lack of access to basic assistive technologies excludes individuals from society, reduces their ability to live independent lives, and is a barrier to the realization of the UN Sustainable Development Goals, which vow “not to leave anyone behind” (MacLachlan 2018). Yet only 10% of the one billion people who require a particular assistive product (wheelchairs, eyeglasses, hearing aids…) do not have access to that life-enabling device, the lack of which is especially poignant within low- and middle-income countries (Albala et al 2021). By 2050, this need is expected to double, due to ageing global populations, increased prevalence of non-communicable diseases, and other factors (ATScale 2020).
Most importantly, already existing conventional evaluation frameworks based on cost-benefit analysis [Drummond et al. 1993, Andrich et al., 1998, Drummond et al., 2015] emphasize the significantly positive economic impact of investment on assistive technology in developed economies, in the form of costs saved to the health and social care systems, compared to profit/value added, or cost recovered: these studies generally find that usage costs of assistive technology, based on historical, modeled, or recently collected data, are lower compared to either standard care costs (Albala et al 2021). Yet such cost-benefit analyses still obfuscate the transformative market-shaping potential that investment on health and assistive technology in particular can unleash on developing economies: not only such studies involve an austerity approach to health investment, but also are difficult to extrapolate to low- and middle-income economies, with very different health systems. Assistive technology provision in those countries has traditionally been conducted in a highly fragmented, erratic, and uncoordinated fashion, through limited public funding, donations of charitable organizations, and small-scale local providers, manufacturing products of varying degrees of quality at a limited price range (ATScale 2020, Savage 2021). Insufficient demand and a low-income base leads investors to view a market as not viable and therefore fail to enter or withdraw from the market, while too much demand with too few suppliers can lead to shortfalls and reduction in quality and reliability; this “market trap” can only be overcome through vigorous market-shaping policy (MacLachlan 2018).
From a dynamic market-shaping perspective that is specifically applied on low- and middle-income economies, we find that sustained provision of assistive technology in those economies has a significant effect on lifetime earning potential in the long run, leading to a 9:1 return on investment in the form of USD 10 trillion in economic benefits over the next 55 years: an average increase of USD 100,000 in income over the life of a child, extended by an average of 1.3 perfect-health years, through improved educational outcomes, better employment and higher productivity, and the reduction of challenges caused by ageing (ATScale 2020).
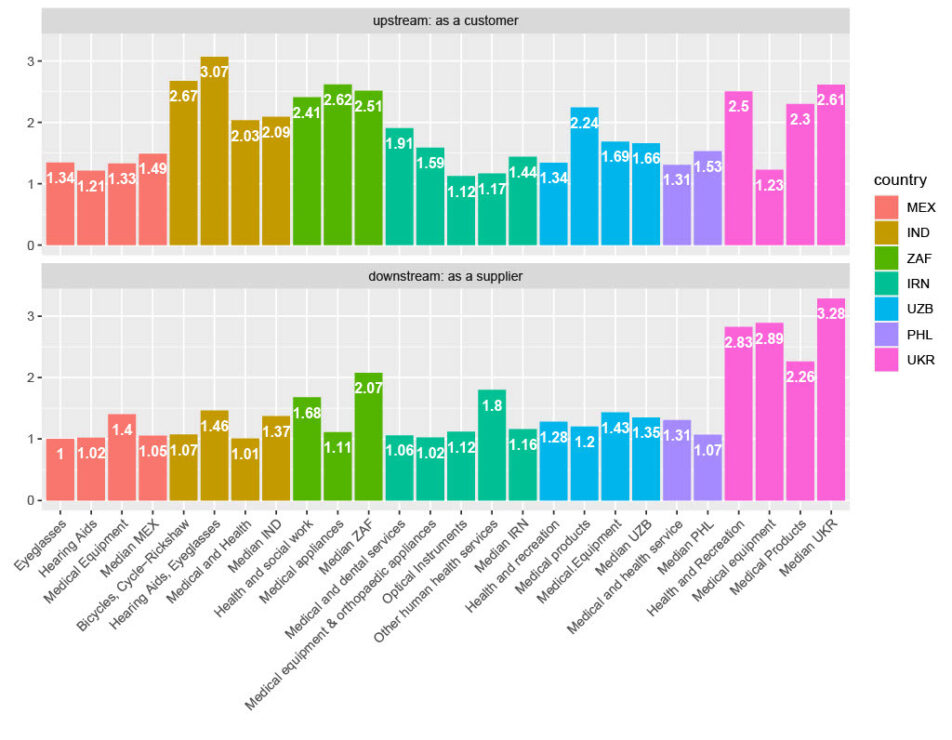
In the short run, the positive spillovers in output and employment of investment per year on health and assistive technology are immediate, rippling through almost all industries (between 75% and 99% of the whole economy) by way of their interdependent linkages in production, while at the same time inducing structural changes in the industrial ecosystem by lowering costs for customers and incentivizing demand for suppliers (Vallès Codina 2022). For instance, the total output multiplier of investment per year can be as high as 307% for the production of hearing aids and ophthalmic goods in India, implying that for each dollar invested an extra 2.07 are gained; for wheelchairs, this number is 267%, in contrast to the average of 209%. Contrary to their conventional view as unimportant or peripheral, health and assistive technology industries are in fact as integral, well connected, and similar as most sectors of the industrial ecosystem, as the input-output production of intermediate goods features a very hierarchical network structure, with few central hubs catering to a wide range of downstream industries producing final goods, among which health and assistive technology are located in the largest structural components.
Acknowledgements
Oriol Vallès Codina, Research Fellow in Innovation Policy, the Institute for Innovation and Public Purpose, AT2030 funded by UK Aid.
References
Albala, S., Holloway, C., Austin, V. and Kattel, R. (2021). New economics of assistive technology: A call for a missions approach. UCL Institute for Innovation and Public Purpose, Working Paper Series (IIPP WP 2021/04). Available at: https://www.ucl.ac.uk/bartlett/public-purpose/wp2021-04
Andrich, R., Ferrario, M., and Moi, M. (1998). A model of cost-outcome analysis for assistive technology. Disability and rehabilitation, 20(1):1–24.
ATscale (2020), The Case for Investing in Assistive Technology, Policy Report.
Drummond, M., Brandt, A., Luce, B., and Rovira, J. (1993). Standardizing economic evaluation methodologies in health care. International Journal of Technology Assessment in Health Care, 9(1):26–36.
Drummond, M. F., Sculpher, M. J., Claxton, K., Stoddart, G. L., and Torrance, G. W. (2015). Methods for the economic evaluation of health care programmes. Oxford University Press.
Kattel, R., Mazzucato, M., Ryan-Collins, J., Sharpe, S. (2018). “The economics of change: Policy appraisal for missions, market shaping and public purpose”. UCL Institute for Innovation and Public Purpose, Working Paper Series (IIPP WP 2018-06). https://www.ucl.ac.uk/bartlett/public-purpose/wp2018-06
MacLachlan, M., McVeigh, J., Cooke, M., Ferri, D., Holloway, C., Austin, V., & Javadi, D. (2018). Intersections between systems thinking and market shaping for assistive technology: the smart (Systems-Market for assistive and related technologies) thinking matrix. International journal of environmental research and public health, 15(12), 2627.
Savage, M., Albala, S., Seghers, F., Kattel, R., Liao, C., Chaudron, M., & Afdhila, N. (2021). Applying market shaping approaches to increase access to assistive technology in low-and middle-income countries. Assistive Technology, 33(sup1), 124-135.
USAID (2014), “Healthy Markets for Global Health: A Market Shaping Primer”, Center for Accelerating Innovation and Impact Policy Report.
Vallès-Codina, O. (2022, forthcoming). “The purely economic case for investing in health for all in lower- and upper-middle income countries: input-output and network analysis of their industrial ecossytem”. UCL Institute for Innovation and Public Purpose, Working Paper Series (IIPP WP 2022-03).
WHO (2021a), “Governing health innovation for the common good”. WHO Council on the Economics of Health for All Brief No. 1 (October 2021)
WHO (2021b), “Financing health for all: Increase, transform, and redirect”. WHO Council on the Economics of Health for All Brief No. 2 (November 2021)